There’s a major reorientation around the patient experience happening in almost every healthcare system in the U.S.
Healthcare leaders and clinicians are coming together to break down organizational silos, increase efficiencies, improve patient outcomes, and, in general, play catch-up to new consumer expectations around “digital experience” that have been formed by platforms like Amazon and Netflix. Leaders are also keenly aware of the emerging “shopability” across many of their services and are eager to mitigate disruption by designing and launching new frictionless digital and analog patient care services that strengthen loyalty to their brand.
However, patient experiences are complex and many teams need help with a way to visualize the totality of the experience (including patient thoughts, feelings, actions, touchpoints, channels, etc.) and “hold it still long enough” so that they can see the spaces in the experience that need attention. This sort of visualization also helps make for some of the significant gaps unaddressed by patient satisfaction surveys.
In response to this need, healthcare organizations are turning to patient journey mapping as a starting point. This turn to mapping makes a lot of sense. When done well, the process is a powerful silo-breaking alignment exercise that helps organizations get the insights they need to focus on the highest value opportunities for transformation across actual patient journeys. These maps then guide actionable strategies that promise a more positive patient experience.
I often hear, however, that, for many teams, patient journey maps don’t live up to their full “insight generation” potential. For a mapping project to be successful, healthcare leaders must aim to obtain the richest data possible; data-driven insights that capture patient expectations, unmet needs, evaluative perceptions, and emotions — these types of insights are often the ones you, me, and patients themselves aren’t aware of prior to research and they can only be learned learned through careful observation.
In this blog, I'll demonstrate issues across common patient journey maps and detail the criteria we use at Highland to design and build effective, patient-focused experiences that increase patient retention and engagement, improve patient satisfaction scores, and in some cases, reach better clinical outcomes.
Not All Patient Journey Maps Are Created Equal
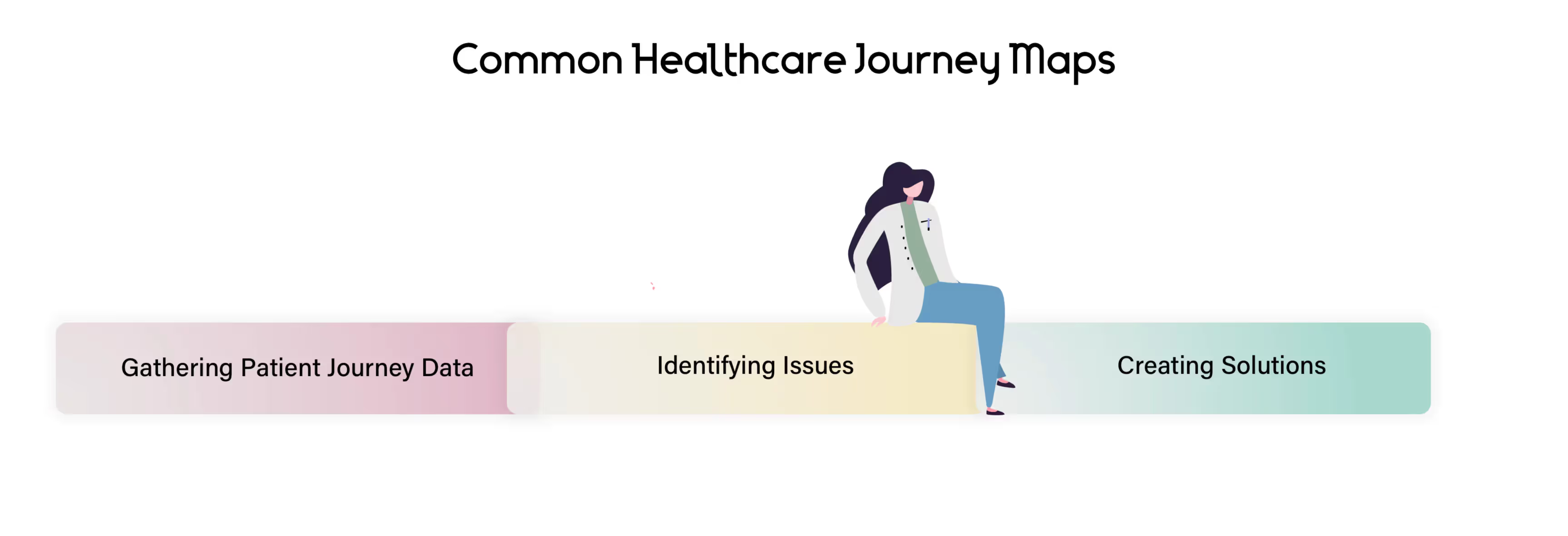
Our observation of many journey maps produced across the healthcare industry is that they just don’t aim high enough. They start with limited goals and insufficient expectations about, “What the map is supposed to do.” This often results in an abundant amount of missed, unidentified, high-impact opportunities.
A mapping process that “doesn’t aim high enough” usually looks something like this:
dedicate ourselves to delivering rich, integrated journey maps. We have a toolbox of dependable methods from the worlds of human-centered design and innovation that go beyond traditional approaches to elicit the more emotive, hard to articulate, true unmet needs of patients, caregivers, and families. This allows us to address those deep unmet functional, social, and emotional needs with targeted intervention strategies, thereby getting to the heart of understanding, improving, and innovating the patient experience.
Our process includes four key elements:
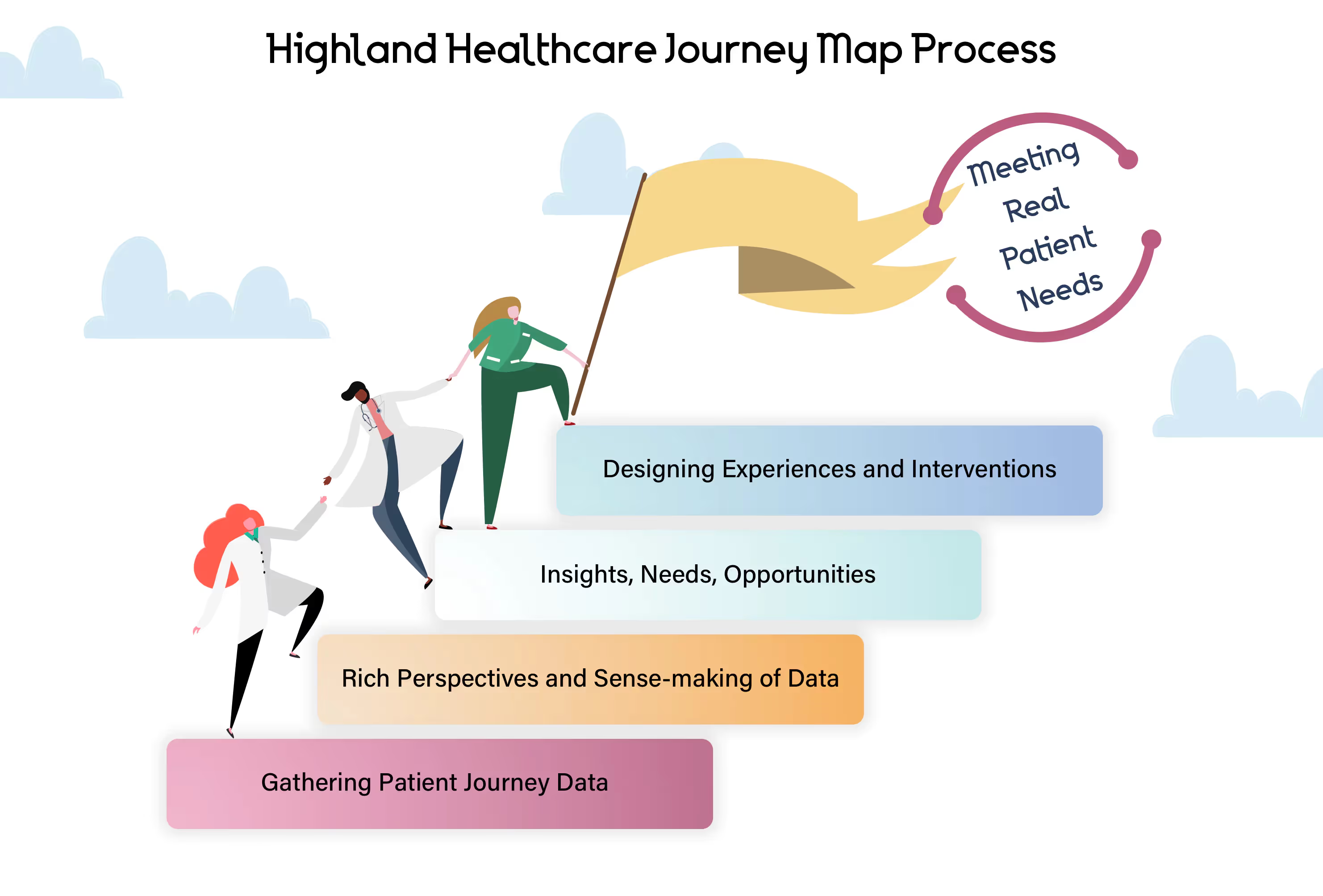
Phase One: Gathering Journey Data
Phase one aims to build a research plan that uncovers patients' needs, hidden desires, and expectations related to your objectives. This includes:
- Healthcare and provider goals: Clearly stating these upfront helps us define a north star for our mapping project. From here, we frame up learning objectives by asking the question, “What must we learn in order to reach these goals?”
- Relevant stakeholders: We need to decide whose journey to map – is it a specific type of patient, a specific care journey, a segment of patients, a potential target customer, care providers, and/or hospital staff? Maps with a clear point-of-view (a clear who, what, and when) are far more likely to be successful than maps hobbled by a diffused focus.
- Research methods: Depending on the learning objectives, we draw upon a variety of exploratory research methods and determine the best set of qualitative research methods to find out what’s really going on.
Once preliminary research is complete, we start capturing insights in a journey map structure.
Phase Two: Rich Perspectives and Sense-Making of Data
This phase is dedicated to making sense of data collected with a rich, expert perspective. Although organizations are reasonably good at gathering data about their patients, data alone fails to communicate the frustrations and experiences. A story can do that, and that’s what we do. Translate data into the patient journey story.
We begin with a series of sorting and clustering to define:
- Stages: How would patients describe the stages of their journey? How different is the way they tell their story from the way a provider or hospital staff member would tell it?
- Actions, mindsets, thoughts, and emotions: Here, we break down behaviors and tasks your patients take, and what they think and feel. It’s impossible to overstate the importance these play because these are essentially key motivators behind every decision your patients make.
- Touchpoints and channels: Touchpoints are times your medical practice and your patients interact — including those you have little to no control over. How do patients experience these touchpoints? Do the existing channels for each touchpoint (the way it is currently delivered) support what the patient needs at that point in their journey?
Phase Three: Insights, Needs, and Opportunities
In phase three, we zoom out to look at the big picture — the themes and patterns that span across patients' entire journey — and transform those into needs, insights, and opportunities. We review:
- Unmet needs: We determine what the patient is actually seeking when they access your services: Are they just seeking a diagnosis and treatment plan? Warm competence like eye contact and empathy? Human connection in the exam room or phone calls with your staff? What are the real needs and motivations that are driving their actions and their evaluation of their care experience?
- Insights: After we take a deep dive into unmet needs, we reveal insights that help us define solutions. Most often, it’s not the quality of care you provide that needs change but instead meeting external factors and emotions that influence patients’ perceptions of that care.
- For example, in a recent mapping project, we looked at the care journey of children born with congenital heart defects. We found that for parents, the journey was actually about their own radical transformation from an “Overwhelmed Survivor” to an “Expert Caregiver”. This transformative frame of mind helped us gain perspective on how and why their needs change dramatically over the course of treatment and, ultimately, how they could become a powerful care team partner by the end of their journey.
- Insights like this give us the clarity and confidence we need to identify high-value opportunities and design tailored interventions.
- Opportunities: Now that we have a rich understanding of the patient journey, we identify opportunities that help create better alignment between your hospital and your patients. This includes but is not limited to staff training, healthcare service design (doctor’s office check-ins, wait times in the waiting room, appointment scheduling) digital transformation (patient portals, mobile apps), internal workflows and processes, marketing (website or social media), care coordination and follow-ups.
Phase Four: Designing Experiences and Interventions
Journey maps shouldn’t just solve a few quick problems. They are meant to provide actionable insights that help you design powerful, patient-focused interventions across the entire experience… even when the patient isn’t physically with you. Most organizations we work with discover gains across:
- Understanding patients: You will learn more about who your patients are, what moves them, and what they care about—giving you deep insight on how to tailor healthcare strategies that meet them where they are and where they expect you to be.
- Understanding your hospital’s ecosystem: Effective journey maps give you an outside-in and inside-out view of your journey, helping you see exactly what internal and external systems, processes, and people are involved.
- Organizational alignment: This exercise brings teams together for shared decision making. We learn and talk through how to resolve specific hurdles impacting the core of your patient experience and align immediately on short and long-term solutions that will drive the most significant impact.
- Strategic investments: No more second guessing. Your patient journey maps become a tool for identifying top priority investments for your organization, bridging across patient portals, provider-patient relationship training, or patient communication workflows.
A Human-Centered Design Framework
No matter the type of healthcare journey you’re improving — primary care, acute care, virtual care — these four phases hold true. Once you learn the interventions that need to take place and build the working team, you’re on your way to improving customer experience for your patients, their families or caregivers, and more.
I believe, “To achieve design-oriented goals, you need design-ready insights.” This means in order to achieve goals like better patient experience, you need insights that enable you to do so. These types of insights can only be derived from human-centered and innovative research techniques — a route Highland takes to be deeply attuned to patients’ deep needs, behaviors, and motivations. In this approach, we can help healthcare organizations like yours design and launch patient-centric experience strategies that further influence better patients' health outcomes and well-being, and overall hospital consumer assessment of healthcare providers and systems (hcahps) scores.
Now that I’ve walked you through all you need to know about patient journey maps, I invite you to begin the process and tell us your goal. Are you looking for process improvements, or are you ready to create high-quality, seamless analog and digital experiences that meet the true unmet needs of your current and new patients?
I agree with you: it should be the latter!